**The information on this page is intended for the use of health and social care professionals only.**
We are proud to be able to provide the UK's only dedicated end of life transport service for patients with support from our St John Ambulance colleagues.
Please note, we are only able to accept bookings for our end of life transport vehicles from healthcare professionals. If you are a member of the public wishing to book one of these vehicles for a family member, please contact your GP to discuss your needs further.
We have three dedicated vehicles, which operate Monday-Friday between 9am-7pm, including bank holidays. The shifts are 9am-5pm, 10am-6pm, and 11am-7pm.
We have produced a video guide for booking an end of life ambulance, which may be used as a teaching aid for healthcare professionals:
Further information
Dying patients have a dedicated service that does not rely on using core NEAS vehicles. This is to enable these patients to die in their place of choice and get there in a timely manner.
To help NEAS allocate the three End of Life vehicles in the most efficient way, please can you read and comply with the following points for booking one of the End of Life Vehicles.
How many end of life vehicles are there?
NEAS have the use of 3 end of life vehicles, operated by St. John Ambulance.
Booking number
Call the urgent line on 0191 414 3144 to book an End of Life vehicle.
Booking times
Monday to Friday 0800-1700, including bank holidays.
Bookings can still be made 24 hours per a day on the normal urgent line but please be aware of the operating times of the three vehicles.
Bookings made outside of these hours will require a core NEAS vehicle so may be more subject to delay.
Operating times
Monday to Friday between 09:00hrs-19:00hrs, including bank holidays
The shifts are 09:00hrs – 17:00hrs, 10:00hrs – 18:00hrs and 11:00hrs – 19:00hrs
Response times
IN HOURS - Monday to Friday 08:00hrs – 17:00hrs - Always booked as a 1 hour response.
OUT OF HOURS – You will be asked if you would like a 1, 2 or 4 hour response.
Appropriate use
- The vehicles will transfer from hospital, hospice or home and can take the patient on their final journey to wherever their chosen place of care/death may be.
- They can transfer from one house to another or one room to another, in the same house
- If a patient stabilises in the hospice and wishes to be discharged home to die, a further journey in the EOL transport will be an appropriate use of this service.
- If the patient is going for treatment or returning from treatment, this is not an appropriate use of this service.
- Please pre-book these journeys via patient transport if own transport is not available.
- Remember, just because the patient is palliative, does not mean this is their final journey, or they are dying and require an End of Life vehicle.
Ready to travel
The patient must be ready, at the time booking e.g. medication, paperwork etc. If they are not, you will be asked to ring back when the patient is ready.
Out of area requests
All out of area requests need to be pre-booked via PTS on 0191 264 8870. Advance notice required. If the patient is being transferred to an area that borders NEAS such as North Yorkshire, Cumbria and the Scottish Borders, these can be booked as normal on the day.
Continuous subcutaneous infusion (CSCI) also known as syringe drivers
All crews can transport patients with a CSCI running. Please be aware our crews aren’t trained to operate them.
Do not attempt cardio-pulmonary resuscitation - DNACPR
If the patient has a DNACPR in place, this must be with the patient for when the crew picks them up.
Most patients will have a DNACPR in place, but it is not a necessity to qualify for the transport.
The section regarding ‘for those individuals transferring to their preferred place of care’ should be completed if the patient is likely to die en route. The crew will still accept the job if it is not completed.
Access and mobility
If a stretcher is requested for the journey, you will be asked the following questions:
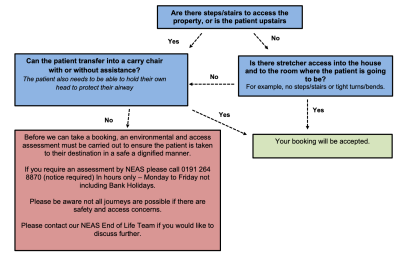
Why is access important?
Without this vital information, a patient could be taken home, and subsequently returned to the hospice or hospital if there is not adequate access. This would be distressing for both the patient and their families, at an already difficult time, and would be a waste of resource. Having this information at the point of call will help ensure patients are transferred to their preferred place of death with dignity and respect.
A recent EOL discharge was refused by the attending crew due to poor access and mobility of a patient. NEAS was not made aware of this, which resulted in a further night’s stay in hospital for the patient, while the family re-arranged the living space by moving the hospital bed downstairs. This could have been avoided if an environmental and access assessment had been carried out prior to the booking.
Setting expectations
Please be aware we have limited vehicles covering this service so delays may occur. If your ambulance is going to be delayed, you will receive a courtesy call from one of our staff to explain the delay and discuss other options.
If you have any queries, please do not hesitate to contact:
- The End of Life Team Team email neas.eolc@nhs.net (Suitable for Patient Identifiable Information)
- End of Life Care Facilitator Karen.Hertwick@neas.nhs.uk 07973694555
- Macmillan Engagement Officer Paul.Galloway@neas.nhs.uk 07976986466
- Macmillan Admin Support Chloe.Ince@neas.nhs.uk 07973767740
For the most up to date advice and guidance, please visit the deciding right website https://northerncanceralliance.nhs.uk/deciding-right/
SPN form version 3 must be completed electronically and sent via email to special.
Please note, this form is for healthcare professional use only.
DNACPRs
Deciding Right is a North-East initiative for making care decisions in advance. All care decisions must come from a shared partnership between the professional, child, young person or adult. But for those who do not have capacity for their choices, or may lose that capacity in the future it is important that the right choices are made.
NEAS should be notified of any advance care planning*, e.g. DNACPR, EHCP’s, etc. A flag can then be added to the patients address to advise call handlers of any decisions identified on the SPN form. The information on the SPN form will support the decision making by NEAS staff, in providing the appropriate response and care, aligning to the patients wishes and preferences.
*Please be aware that special patient notes, is not just for advance care decisions. See form for details.
DNACPR flags will remain valid on our system until:
- The patient dies,
- Moves out of the NEAS geographical area
- The DNACPR is rescinded (NEAS must be notified of this)
NEAS are hopeful that these changes will promote robust information sharing. Most importantly, ensuring patients advance care decisions are known and respected, and also reducing repetition in completion of SPNs.
